This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Case:
A 50 yr old male who is daily wage labourer by occupation came to the casualty with c/o sweeling of the legs upto the Knee since 2 months, SOB since 1month, decreased urine output since 20 days , abdominal distension since 20 days.
HOPI:
He was apparently asymptomatic 2months ago then he developed Abdominal distension which was gradually progressive 6 days later he also noticed swelling of his legs which was gradually progressive extending upto the knee (pedal edema-soft and pitting type) and then he developed puffiness of his face 20days back, decreased urinary output and burning micturation since 20 days and chest pain on and off since 20days which is squeezing type of pain usually during night wakes up and walks for a while for it relieve, pain was non radiating and not a/w sweating or giddiness, sob since 20days(he couldn't walk for long distance and wakes up in the middle of the Sleep d/t severe dyspnea"grade 3-4")a/w orthopnea and PND.
Patient went to an outside hospital where he was put on foleys -clear urine f/b hematuria- present.
past history :
k/c/o DM on OHA's (unkown) since 3 years.
not a k/c/o HTN, Asthma, Epilepsy, CAD.
h/o polio at 6years of age d/t which he developed deviation of mouth to the left and right lower limbs paralysis.
personal history:
Diet- mixed
Appetite-normal
Bowel movements-regular
Bladder-decreased
addictions- alcohol 1-2 times/week (90ml ) since 20yrs
smoking: 1 pack/day (10/day) - beedi since 30yrs
General Examination:
Patient is conscious, coherant, cooperative
Oriented to time place and person
Pedal edema-B/L pedal edema which is soft and of pitting type.
no pallor ,icterus,cyanosis , clubbing, lymphadenopathy
Vitals:
temp: 98⁰F
pulse : 100/min
respiration: 22 /min
BP left arm : 110/70 mmhg
sp02: 98%
GRBS: 177 mg/dl
Systemic examination:
CVS-
Inspection:
Chest wall- symmetrical
No Precordial bulge, Pectus carinatum/excavatum
scar, No sinuses
Apical impulse present.
JVP: Elevated.
Parasternal heaves absent.
Palpation:
Apical impulse- localized and present in the 6th intercostal space feltat anterior axillary line.
Auscultation:
Pansystolic murmur(S1- faintly heard), S2 heard.
Respiratory system-BAE+ IAA ans ISA crepitations.
Abdomen-
- shape - obese
- soft,and non tender
- Bowel sounds heard.
CNS- NFD
provisional diagnosis:
Dialated cardiomyopathy secondary to ?CAD
ejection fraction 28 %
Investigations:
USG abdomen-
X Ray chest PA view:
ECG-
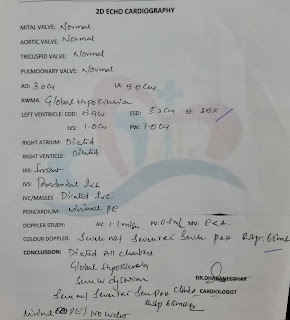
2D echo heart:
Treatment:
1)propped up position
2)fluid restriction to <1lit /day
3)salt restriction <2g/day
4inj lasix 80mg in 50ml ns @5ml/hr
5)inj dobutamine250mcg in 50ml ns @3.6ml/hr
6)tab ecosprin av 75/20mg /po/od
7)grbs 6th hourly premeal
8) inj hai s/c tid
9)syp cremaffin plus 10ml/po/hs
10) avoid strenuous activity.








Comments
Post a Comment