A 65year old with Decreased urinary output and puffiness of face,Bilateral pedal edema and abdominal distension
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CASE:
A 65 year old man who used be farmer resident of anantharam came to the opd with chief complaints of decreased urine output since 15 days and puffiness of face , abdominal distension and pedal edema since 15days.
History of present illness:
Patient was apparently asymptomatic 1year back then he noticed puffiness of face and pedal edema(pitting type)and went to local rmp and treated conservatively and she also noticed that his wounds on the foot were not healing so went to a local hospital and diagnosed to have diabetes 1 year back and is on medication (unknown). From 1 year he has been having puffiness of face ,pedal edema on and off for which he is being treated conservatively by local RMP since 20 days patient is complaining of burning micturation and puffiness of face and pedal edema and abdominal distension and from the last 15 days there is decreased urine output(when he tries to micturate only few drops of urine comes out). 5 days back when they are going to hospital and had one episode of vomiting and developed shortness of breath Grade 1.he was put a central line and underwent dialysis on 6-8-2022.
Past history:
He is a known case of Hypertension from 3years and was on medication.(unknown)
He is also a known case of diabetes mellitus from 1 year and is on medication (unknown).
He had an RTA 3 years back had an injury on the left side of thorax and managed accordingly.
He is not a known case of asthma, epilepsy, TB, CAD.
Personal history:
Diet-mixed
Appetite-decreased since 15 days.
Sleep-adequate
Bladder movements-decreased
Bowel-no stools since 15 days
Addictions-alcohol since past 40 years (90ml).
Family history:Not significant
Treatment history: History of usage of antihypertensive and oral antidiabetic medication.
General examination:
Patient is conscious coherant cooperative
Moderately built and moderately nourished
Pallor-absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Generalised lymphadenopathy-absent
Pedal edema-present (pitting type) grade 2.
Vitals :
Temperature-99 degree F
Pulse rate-110 bpm
Respiratory rate-24cpm
Blood pressure -130/90mm of hg
Spo2-90%at room air and 98%at 4 liters of O2
Grbs-112mg /dl
Systemic examination:
Per abdomen:
Inspection:
Abdominal distended
No scars or sinuses
No dilated veins
Umblicus everted
Palpation:
Firm and tender over the left hypochondrium.
Percussion:
Tympanic note in all quadrants.
Auscultation:Bowel sounds heard
Cardiovascular system:
S1 and S2 heard no murmurs heard. JVP Raised
Respiratory system:
Bilateral air entry-present,vesicular breath sounds-heard
Central nervous system:
No focal neurological deficit, cranial nerves-intact.
Provisional diagnosis:
AKI (post renal)?
Investigations:
Abdomen and KUB scan on 4-8-2022:
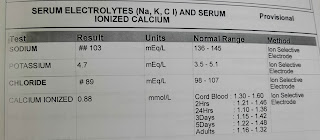
On 5-8-2022
On 6-8-2022:
At5:47pm
At 5:47am
At12:07pm
At 12:07pm
ECG on 5-8-2022:
Treatment:
On 5-8-2022:
Inj. LASIX 40mg I.v Stat.
On 6-8-2022:
Tab. NADOSIS 500mg P.o BD
Tab. SHELCAL P.o OD
Inj. 3%NaCl at 8ml/hr on flow.























Comments
Post a Comment